Abstract

Background:
The median age at diagnosis of myeloproliferative neoplasms (MPN) is in the sixth decade, though adolescents and young adults (AYA) with MPN comprise a distinct, growing sub-population. Preliminary data has exposed a unique phenotype and clinical trajectory in these patients (Haematologica. 2019; 104(8):1580-1588; Am J Hematol. 2018; 93(12):1474-1484). Additional questions remain concerning the biological underpinnings of this population, but also, importantly, patterns of care and outcomes in the real-world setting. The objective of this study was to systematically evaluate patterns of care (diagnosis and management), as well as complications in AYA with MPN.
Methods:
Patients were recruited from the registry of the GQR LMC-NMP, an extensive provincial MPN network (>11 academic and community centers across Quebec). AYA were age 18-40 years at diagnosis (control population, > 40 years at diagnosis), diagnosed between 1978 and 2019 adhering to World Health Organization criteria, with exemption of bone marrow sampling in a subset. Standard risk stratification was according to MPN subtype. Conventional statistical methods were used for analyses (JMP® Pro 14.1.0 software; SAS Institute, Cary, NC, USA).
Results:
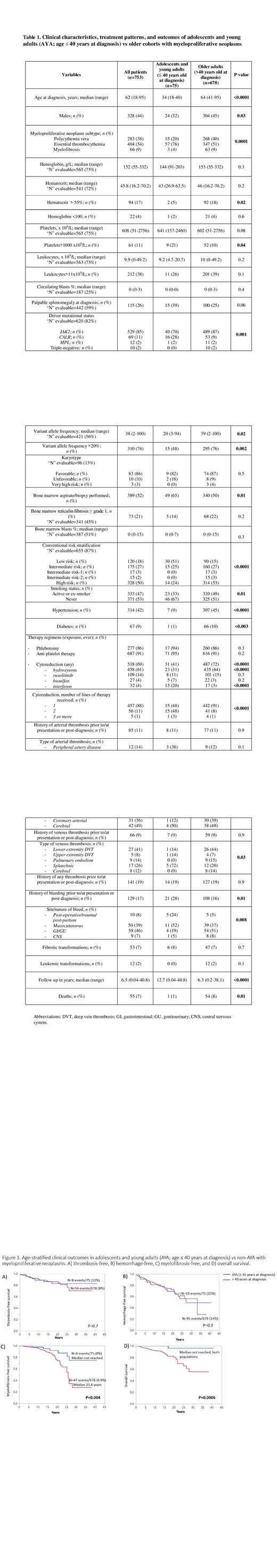
The AYA population consisted of 75 patients: n=15 (20%) polycythemia vera (PV), n=57 (76%) essential thrombocythemia (ET), and n=3 (4%) myelofibrosis (Table 1). Corresponding MPN subtypes in patients > 40 years were 268 (40%) PV, 347 (51%) ET, and 63 (9%) MF. Median age at diagnosis was 34 years (range 18-40) in AYA vs 64 (41-95) in the older cohort. AYA were predominantly female (68% vs 55%; p=0.03). Median platelet count at diagnosis was higher in AYA vs non-AYA (641 vs 602 x10 9/L; p=0.08), with a greater proportion of patients (21% vs 10%; p=0.04) presenting with platelets > 1000 x10 9/L. A trend towards more frequent palpable splenomegaly was observed in AYA (39% vs 25%; p=0.06). Driver mutation status in AYA vs older adults, respectively, was JAK2 (70% vs 87%) followed by CALR (28% vs 9%), MPL (2% in both), and triple negative (0% vs 2%) (p=0.001). Variant allele frequency (VAF) was significantly lower in AYA with median (range) of 20% (3-94) vs 39% (2-100) in non-AYA (p=0.02), with fewer AYA presenting VAF > 20% at diagnosis (48% vs 76%; p=0.002). Risk stratification disclosed 24% of AYA (n=14) vs 53% (n=314) of non-AYA subjects to be high risk (p<0.0001). Significantly fewer cardiovascular co-morbidities were reported in AYA (p<0.003).
Regarding work-up and management, markedly more AYA patients underwent bone marrow sampling vs older patients (65% vs 50%; p=0.01). While similar rates of phlebotomy and anti-platelet administration were reported (p=0.3 and 0.2, respectively), appreciably fewer AYA patients were treated with cytoreductive agents (41% vs 72% non-AYA, p<0.0001). The nature of cytoreductive therapy varied between AYA vs older subgroups (p<0.0001 for both hydroxyurea and interferon). A greater proportion of AYA (51%) vs non-AYA (9%) were also exposed to 2+ lines of cytoreduction (p<0.0001).
Similar rates of both arterial and venous thrombosis prior to/at diagnosis or post-diagnosis were found across AYA and non-AYA cohorts (p=0.9). Sites of predilection of venous events, however, were distinctive: AYA exhibited a preponderance of splanchnic vein and upper extremity thrombosis (72% and 14% respectively) vs non-AYA (20% and 7%) (p=0.03). Rates of hemorrhagic complications were significantly higher in AYA vs older adults (28% vs 16%; p=0.01), with distinctive patterns of bleeding, dominated by post-procedural/trauma/post-partum (24%) and mucocutaneous (52%) in AYA vs non-AYA (p=0.008).
Kaplan-Meier survival analyses revealed proportional rates of thrombosis and hemorrhage-free survival but longer myelofibrosis-free (p=0.004) and overall survival (p=0.0006) in AYA vs older adults (Figure 1).
Conclusions:
AYA with MPN not only display unique clinical features but are also subject to distinct diagnostic and management practices. More rigorous investigational approaches and a propensity to address AYA with intensive cytoreductive strategies may reflect a signal of overtreatment of this population. Further, the incidence and nature of thrombotic/bleeding complications show distinctive patterns in AYA, requiring targeted vigilance and an individualized approach to monitoring and therapy.
Szuber: Novartis: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal